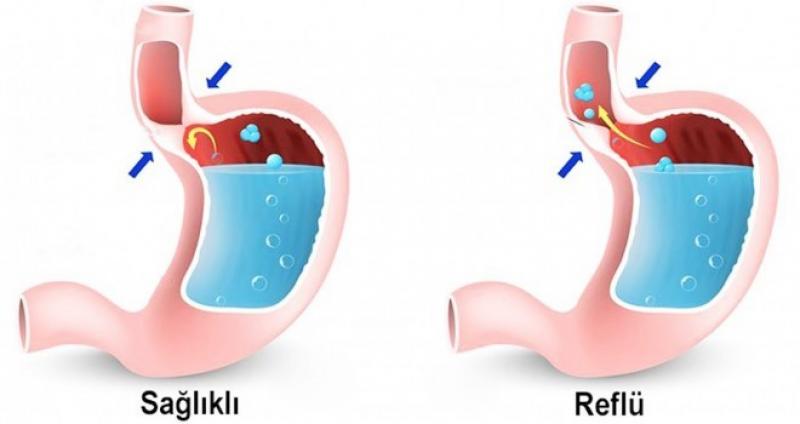
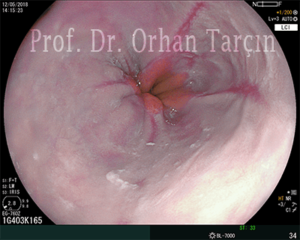
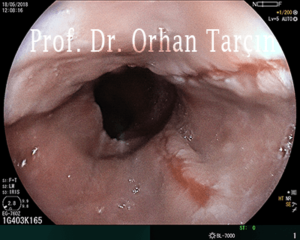
Gastroesophageal reflux disease (GERD) occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (esophagus). This backwash (acid reflux) can irritate the lining of your esophagus. GERD itself is not a disease and occurs multiple times each day without producing symptoms or mucosal damage. In contrast, GERD is a spectrum of disease usually producing symptoms of heartburn and acid regurgitation. GERD is a consequence of the failure of the normal antireflux barrier to protect against frequent and abnormal amounts of refluxed material. Most patients have no visible mucosal damage at the time of endoscopy, whereas others have esophagitis, peptic strictures, or Barrett’s esophagus.
Symptoms
Common signs and symptoms of GERD include:
• A burning sensation in your chest (heartburn), usually after eating, which might be worse at night
• Chest pain
• Difficulty swallowing
• Regurgitation of food or sour liquid
• Sensation of a lump in your throat
If you have nighttime acid reflux, you might also experience:
• Chronic cough
• Laryngitis
• New or worsening asthma
• Disrupted sleep
Causes
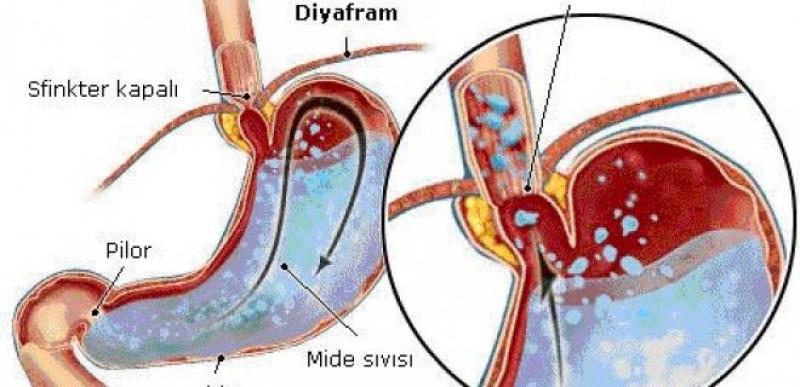
GERD is caused by frequent acid reflux. When you swallow, a circular band of muscle around the bottom of your esophagus (lower esophageal sphincter) relaxes to allow food and liquid to flow into your stomach. Then the sphincter closes again.
If the sphincter relaxes abnormally or weakens, stomach acid can flow back up into your esophagus. This constant backwash of acid irritates the lining of your esophagus, often causing it to become inflamed.
• Self-help
Diet and lifestyle changes are the foundation for treating the symptoms of reflux:
• Eat smaller meals. A large meal remains in the stomach for several hours, increasing the chances for reflux. Eat several small meals throughout the day, rather than three large meals.
• Relax when you eat. Stress increases the production of stomach acid. Make meals a pleasant, relaxing experience. Sit down. Eat slowly. Chew completely. Play soothing music.
• Relax between meals. Relaxation therapies such as deep breathing, meditation, massage, tai chi, or yoga may help prevent and relieve heartburn.
• Remain upright after eating. Remain upright for at least three hours after eating. During this time, don’t bend over, strain to lift heavy objects, or lie down.
• Avoid eating within three hours of going to bed. Do not eat just before bedtime.
• Lose weight, if needed. Extra pounds increase pressure on the stomach and can push acid into the esophagus.
• Loosen up. Avoid tight belts, waistbands, and other clothing that puts pressure on your stomach.
• Avoid foods that burn. Avoid foods that can trigger reflux.
These include:
• high-fat foods
• spicy dishes
• tomatoes and tomato products
• citrus fruits
• garlic and onions
• milk
• carbonated drinks
• coffee (including decaf) and tea
• chocolate
• mints
• alcohol
• Don’t smoke. Nicotine stimulates stomach acid and affects the function of the lower esophageal sphincter.
• Chew gum. This increases saliva production, soothing the esophagus and washing acid back down to the stomach.
• Ask your doctor about your medications. Certain drugs can cause heartburn. These include aspirin and other nonsteroidal anti-inflammatory drugs, oral contraceptives, estrogen therapy, narcotics, certain antidepressants, and some asthma medications.
• Raise the head of your bed. If you’re bothered by nighttime heartburn, elevate the head of your bed by placing a wedge (available in medical supply stores) under your upper body. Don’t elevate your head with extra pillows. That makes reflux worse by bending you at the waist and compressing your stomach.
• Exercise wisely. Wait at least two hours after a meal before exercising.
Health Risk Factors
Many adults experience heartburn and anyone at any age can develop GERD. Here are some factors that may increase your risk:
• Scleroderma: This autoimmune disorder, in which the immune system attacks healthy cells in the body, increases your risk for GERD. Many people with this concern also have GERD because the esophagus is the most commonly affected organ in scleroderma.
• Asthma and COPD: Again, experts aren’t sure which is the chicken or the egg when it comes to asthma and GERD, but most agree there is an important connection. In addition to the aforementioned concerns, GERD has been associated with a number of other upper respiratory problems and may be a cause of asthma that starts in adulthood, rather than a result.
• Chronic obstructive pulmonary disease (COPD): also puts you at a higher risk of developing GERD, and having GERD may make your COPD symptoms worse.
• Diabetes: People with diabetes, especially type 1 diabetes, often develop a condition called gastroparesis. This condition is characterized by delayed stomach emptying. The pressure within the stomach can increase, which in turn can result in reflux, making you more prone to develop GERD.
• Celiac Disease: People with celiac disease seem to have a much higher rate of GERD than the general population, especially when they’re newly diagnosed. Studies have shown that a gluten-free diet significantly reduces symptoms of GERD. Experts aren’t sure whether consuming gluten causes GERD or if GERD is an associated condition of celiac disease. Sometimes GERD doesn’t occur until after a person is diagnosed with celiac disease, which indicates that there may be something else causing it.