What is constipation?
Constipation is a condition in which a person has uncomfortable or infrequent bowel movements. Generally, a person is considered to be constipated when bowel movements result in passage of small amounts of hard, dry stool, usually fewer than three times a week. However, normal stool elimination may consist of having a bowel movement three times a day or three times a week; it depends on the person.
 Treatment for chronic constipation depends in part on the underlying cause. However, in some cases, a cause is never found.
Treatment for chronic constipation depends in part on the underlying cause. However, in some cases, a cause is never found.
Symptoms
What are the symptoms of constipation? The following are the most common symptoms of constipation. However, each individual may experience symptoms differently. Symptoms may include:
• Difficult and painful bowel movements
• Bowel movements fewer than three times a week
• Feeling bloated or uncomfortable
• Feeling sluggish
• Abdominal pain

What causes constipation?
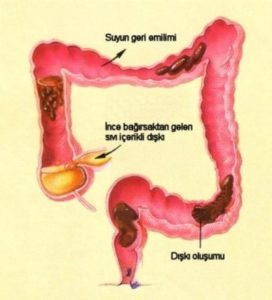
Hard, dry stools are the result of the colon absorbing too much water. Normally, as food moves through the colon (also known as the large intestine) the colon absorbs water while forming stool (waste products). Muscle contractions then push the stool toward the rectum, and, by the time the stool reaches the rectum, most of the water has been absorbed, making the stool solid.
• Lack of exercise: People who exercise regularly generally don’t develop constipation. Basically, the colon responds to activity. Good muscle tone in general is important for regular bowel movements. The abdominal wall muscles and the diaphragm all play a crucial role in the process of defecation. If these muscles are weak, they’re not going to be able to do the job as well. But exercise is not a cure-all. Increasing exer-cise to improve constipation may be more effective in older people, who tend to be more sedentary, than in younger people.
• Opioids: The digestive tract has receptors for opioids, and constipation can occur (or worsen) when people take opioid pain medications. Opioid-induced constipation occurs in roughly 94% of cancer patients taking opioids for pain and 41% of people taking opioids for chronic noncancer pain.
• Other medications: Constipation is a side effect of many prescription and over-the-counter drugs. These include antacids that contain aluminum, antispasmodics, antidepressants, tranquilizers and sedatives, bismuth salts, iron supplements, diuretics, anticholinergics, calcium-channel blockers, and anticonvulsants.
• Irritable bowel syndrome (IBS): Some people who suffer from IBS have sluggish bowel movements, straining during bowel movements, and abdominal discomfort. Constipation may be the predominant symptom, or it may alternate with diarrhea. Cramping, gas, and bloating are also common.
• Abuse of laxatives: Laxatives are sometimes used inappropriately, for example, by people suffering from anorexia nervosa or bulimia. But for people with long-term constipation, the extended use of laxatives may be a reasonable solution. In the past, long-term use of some laxatives was thought to damage nerve cells in the colon and interfere with the colon’s innate ability to contract. However, newer formulations of laxatives have made this outcome rare.
• Changes in life or routine: Traveling can give some people problems because it disrupts normal diet and daily routines. Aging often affects regularity by reducing intestinal activity and muscle tone. Pregnancy may cause women to become constipated because of hormonal changes or because the enlarged uterus pushes on the intestine.
• Ignoring the urge: If you have to go, go. If you hold in a bowel movement, for whatever reason, you may be inviting a bout of constipation. People who repeatedly ignore the urge to move their bowels may eventually stop feeling the urge.
• Not enough fiber and fluids in the diet: A diet too low in fiber and fluids and too high in fats can con-tribute to constipation. Fiber absorbs water and causes stools to be larger, softer, and easier to pass. Increasing fiber intake helps cure constipation in many people, but those with more severe constipation sometimes find that increasing fiber makes their constipation worse and leads to gassiness and discomfort.
• Other causes: Diseases that can cause constipation include neurological disorders, such as Parkinson’s disease, spinal cord injury, stroke, or multiple sclerosis; metabolic and endocrine disorders, such as hypothyroidism, diabetes, or chronic kidney disease; bowel cancer; and diverticulitis. A number of systemic conditions, like scleroderma, can also cause constipation. In addition, intestinal obstructions, caused by scar tissue (adhesions) from past surgery or strictures of the colon or rectum, can compress, squeeze, or narrow the intestine and rectum, causing constipation.
Risk factors
Factors that may increase your risk of chronic constipation include:
• Being an older adult
• Being a woman
• Being dehydrated
• Eating a diet that’s low in fiber
• Getting little or no physical activity
• Taking certain medications, including sedatives, narcotics, some antidepressants or medications to lower blood pressure
• Having a mental health condition such as depression or an eating disorder
Prevention
The following can help you avoid developing chronic constipation:
• Include plenty of high-fiber foods in your diet, including beans, vegetables, fruits, whole grain cereals and bran.
• Eat fewer foods with low amounts of fiber such as processed foods, and dairy and meat products.
• Drink plenty of fluids.
• Stay as active as possible and try to get regular exercise.
• Try to manage stress.
• Don’t ignore the urge to pass stool.
• Try to create a regular schedule for bowel movements, especially after a meal.
• Make sure children who begin to eat solid foods get plenty of fiber in their diets.
How is constipation diagnosed?
The tests performed by a doctor will depend on the duration and severity of the constipation, since most persons experience constipation at one time or another. The doctor will also take into account the patient’s age, and whether there is blood in the stool, recent changes in bowel habits, or weight loss.
Diagnosing constipation may include:
• Medical history. The doctor will ask for a description of the constipation, including duration of symptoms, frequency of bowel movements, and other information to help determine the cause of the constipation.
• Physical examination. A physical examination may also include a digital rectal examination (DRE), in which the doctor inserts a gloved, lubricated finger into the rectum to evaluate the tone of the muscle that closes off the anus. This examination also helps detect tenderness, obstruction, blood, amount and caliber of stool, and if enlargement of the rectum is present.
Other diagnostic tests may include:
• Abdominal X-ray
• Lower GI (gastrointestinal) series (also called barium enema): A lower GI series is a procedure that examines the rectum, the large intestine, and the lower part of the small intestine. A fluid called barium (a metallic, chemical, chalky, liquid used to coat the inside of organs so that they will show up on an X-ray) is given into the rectum as an enema. An X-ray of the abdomen shows strictures (narrowed areas), obstructions (blockages), and other problems.
• Colonoscopy: Colonoscopy is a procedure that allows the doctor to view the entire length of the large intestine, and can often help identify abnormal growths, inflamed tissue, ulcers, and bleeding. It involves inserting a colonoscope, a long, flexible, lighted tube, in through the rectum up into the colon. The colonoscope allows the doctor to see the lining of the colon, remove tissue for further examination, and possibly treat some problems that are discovered.
• Sigmoidoscopy: A sigmoidoscopy is a diagnostic procedure that allows the doctor to examine the inside of a portion of the large intestine, and is helpful in identifying the causes of diarrhea, abdominal pain, constipation, abnormal growths, and bleeding. A short, flexible, lighted tube, called a sigmoidoscope, is inserted into the intestine through the rectum. The scope blows air into the intestine to inflate it and make viewing the inside easier.
• Colorectal transit study: This test shows how well food moves through the colon. The patient swallows capsules containing small markers which are visible on X-ray. The patient follows a high-fiber diet during the course of the test, and the movement of the markers through the colon is monitored with abdominal X-rays taken several times three to seven days after the capsule is swallowed.
• Anorectal function tests: These tests diagnose constipation caused by an abnormal functioning of the anus or rectum.
Treatment for constipation
Specific treatment for constipation will be determined by your doctor based on:
• Your age, overall health, and medical history
• Extent of the condition
• Your tolerance for specific medications, procedures, or therapies
• Expectations for the course of this condition
Most often, constipation can be treated through dietary and lifestyle changes, which relieve symptoms and help prevent the condition. Treatment may include:
• Increase your fiber intake: Adding fiber to your diet increases the weight of your stool and speeds its passage through your intestines. Slowly begin to eat more fresh fruits and vegetables each day. Choose whole-grain breads and cereals. Your doctor may recommend a specific number of grams of fiber to consume each day. In general, aim for 14 grams of fiber for every 1,000 calories in your daily diet. A sudden increase in the amount of fiber you eat can cause bloating and gas, so start slowly and work your way up to your goal over a few weeks.
• Exercise most days of the week: Physical activity increases muscle activity in your intestines. Try to fit in exercise most days of the week. If you do not already exercise, talk to your doctor about whether you are healthy enough to start an exercise program.
• Don’t ignore the urge to have a bowel movement: Take your time in the bathroom, allowing yourself enough time to have a bowel movement without distractions and without feeling rushed.
• Laxatives: Laxatives may be prescribed after diet and lifestyle changes have failed to be effective.
• Training your pelvic muscles
• Biofeedback training: involves working with a therapist who uses devices to help you learn to relax and tighten the muscles in your pelvis. Relaxing your pelvic floor muscles at the right time during defecation can help you pass stool more easily. During a biofeedback session, a special tube (catheter) to measure muscle tension is inserted into your rectum. The therapist guides you through exercises to alternately relax and tighten your pelvic muscles. A machine will gauge your muscle tension and use sounds or lights to help you understand when you’ve relaxed your muscles.