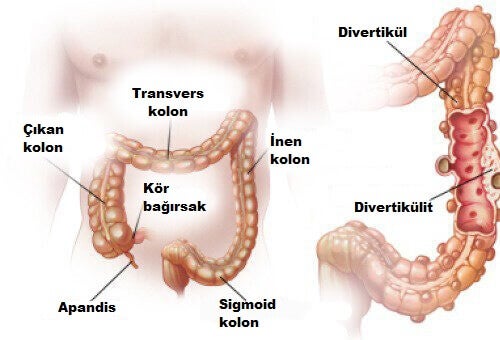
Diverticula are small, bulging pouches that can form in the lining of your digestive system. They are found most often in the lower part of the large intestine (colon). Diverticula are common, especially after age 40, and seldom cause problems.
Sometimes, however, one or more of the pouches become inflamed or infected. That condition is known as diverticulitis (die-vur-tik-yoo-LIE-tis). Diverticulitis can cause severe abdominal pain, fever, nausea and a marked change in your bowel habits.
Mild diverticulitis can be treated with rest, changes in your diet and antibiotics. Severe or recurring diverticulitis may require surgery.
Symptoms
The signs and symptoms of diverticulitis include:
- Pain, which may be constant and persist for several days. The lower left side of the abdomen is the usual site of the pain. Sometimes, however, the right side of the abdomen is more painful, especially in people of Asian descent.
- Nausea and vomiting.
- Fever.
- Abdominal tenderness.
- Constipation or, less commonly, diarrhea.
Causes
Diverticula usually develop when naturally weak places in your colon give way under pressure. This causes marble-sized pouches to protrude through the colon wall.
Diverticulitis occurs when diverticula tear, resulting in inflammation or infection or both.
Risk factors
Several factors may increase your risk of developing diverticulitis:
- Aging: The incidence of diverticulitis increases with age.
- Obesity: Being seriously overweight increases your odds of developing diverticulitis.
- Smoking: People who smoke cigarettes are more likely than nonsmokers to experience diverticulitis.
- Lack of exercise: Vigorous exercise appears to lower your risk of diverticulitis.
- Diet high in animal fat and low in fiber: A low-fiber diet in combination with a high intake of animal fat seems to increase risk, although the role of low fiber alone isn’t clear.
Prevention
To help prevent diverticulitis:
• Exercise regularly: Exercise promotes normal bowel function and reduces pressure inside your colon. Try to exercise at least 30 minutes on most days.
• Eat more fiber: A high-fiber diet decreases the risk of diverticulitis. Fiber-rich foods, such as fresh fruits and vegetables and whole grains, soften waste material and help it pass more quickly through your colon. Eating seeds and nuts isn’t associated with developing diverticulitis.
• Drink plenty of fluids: Fiber works by absorbing water and increasing the soft, bulky waste in your colon. But if you don’t drink enough liquid to replace what’s absorbed, fiber can be constipating.
Complications
About 25 percent of people with acute diverticulitis develop complications, which may include:
• An abscess, which occurs when pus collects in the pouch.
• A blockage in your colon or small intestine caused by scarring.
• An abnormal passageway (fistula) between sections of bowel or the bowel and bladder.
• Peritonitis, which can occur if the infected or inflamed pouch ruptures, spilling intestinal contents into your abdominal cavity. Peritonitis is a medical emergency and requires immediate care.
Treatment
Treatment depends on the severity of your signs and symptoms.
Uncomplicated diverticulitis
• If your symptoms are mild, you may be treated at home. Your doctor is likely to recommend:
• Antibiotics to treat infection, although new guidelines state that in very mild cases, they may not be needed.
• A liquid diet for a few days while your bowel heals. Once your symptoms improve, you can gradually add solid food to your diet.
• An over-the-counter pain reliever, such as acetaminophen (Tylenol, others).
• This treatment is successful in most people with uncomplicated diverticulitis.
Complicated diverticulitis
• If you have a severe attack or have other health problems, you’ll likely need to be hospitalized. Treatment generally involves:
• Intravenous antibiotics
• Insertion of a tube to drain an abdominal abscess, if one has formed
Surgery
You’ll likely need surgery to treat diverticulitis if:
- You have a complication, such as a bowel abscess, fistula or obstruction, or a puncture (perforation) in the bowel wall
- You have had multiple episodes of uncomplicated diverticulitis
- You have a weakened immune system
There are two main types of surgery:
• • Primary bowel resection. The surgeon removes diseased segments of your intestine and then reconnects the healthy segments (anastomosis). This allows you to have normal bowel movements. Depending on the amount of inflammation, you may have open surgery or a minimally invasive (laparoscopic) procedure.
• • Bowel resection with colostomy. If you have so much inflammation that it’s not possible to rejoin your colon and rectum, the surgeon will perform a colostomy. An opening (stoma) in your abdominal wall is connected to the healthy part of your colon. Waste passes through the opening into a bag. Once the inflammation has eased, the colostomy may be reversed and the bowel reconnected.
Follow-up care
Your doctor may recommend colonoscopy six weeks after you recover from diverticulitis, especially if you haven’t had the test in the previous year. There doesn’t appear to be a direct link between diverticular disease and colon or rectal cancer. But colonoscopy — which isn’t possible during a diverticulitis attack — can exclude colon cancer as a cause of your symptoms.
After successful treatment, your doctor may recommend surgery to prevent future episodes of diverticulitis. The decision on surgery is an individual one and is often based on the frequency of attacks and whether complications have occurred.