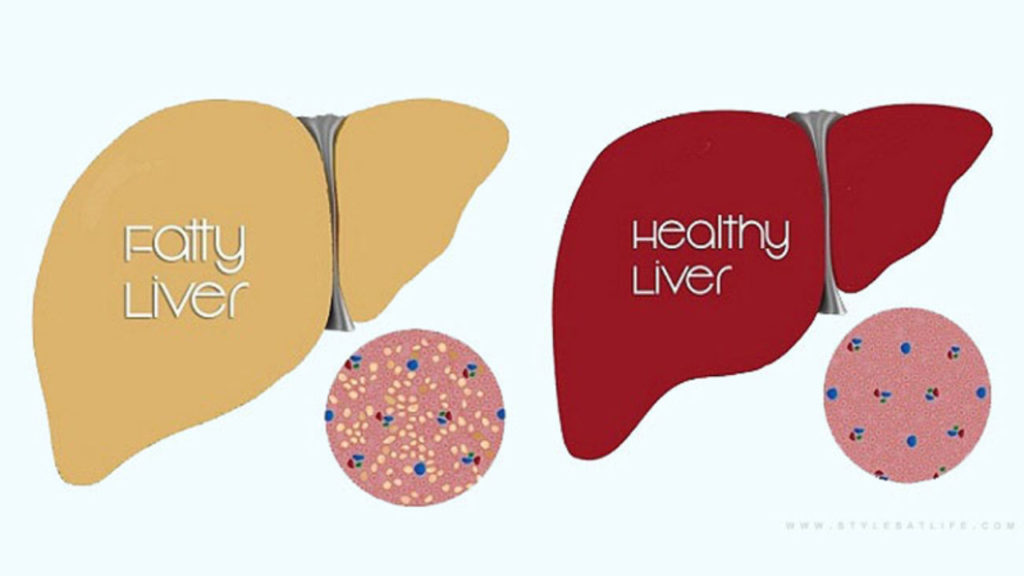
Fatty liver is also known as hepatic steatosis. It happens when fat builds up in the liver. Having small amounts of fat in your liver is normal, but too much can become a health problem.
Your liver is the second largest organ in your body. It helps process nutrients from food and drinks and filters harmful substances from your blood. Nonalcoholic steatohepatitis, a potentially serious form of the disease, is marked by liver inflammation, which may progress to scarring and irreversible damage. This damage is similar to the damage caused by heavy alcohol use. At its most severe, nonalcoholic steatohepatitis can progress to cirrhosis and liver failure.
Nonalcoholic fatty liver disease occurs in every age group but especially in people in their 40s and 50s who are at high risk of heart disease because of such risk factors as obesity and type 2 diabetes. The condition is also closely linked to metabolic syndrome, which is a cluster of abnormalities including increased abdominal fat, poor ability to use the hormone insulin, high blood pressure and high blood levels of triglycerides, a type of fat.
Symptoms
Nonalcoholic fatty liver disease usually causes no signs and symptoms. When it does, they may include:
• Enlarged liver
• Fatigue
• Pain in the upper right abdomen
Possible signs and symptoms of nonalcoholic steatohepatitis and cirrhosis (advanced scarring) include:
• Abdominal swelling (ascites)
• Enlarged blood vessels just beneath the skin’s surface
• Enlarged breasts in men
• Enlarged spleen
• Red palms
• Yellowing of the skin and eyes (jaundice)
Causes
Experts don’t know exactly why some people accumulate fat in the liver while others do not. Similarly, there is limited understanding of why some fatty livers develop inflammation that progresses to cirrhosis. Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis are both linked to the following:
• Overweight or obesity
• Insulin resistance, in which your cells don’t take up sugar in response to the hormone insulin
• High blood sugar (hyperglycemia), indicating prediabetes or actual type 2 diabetes
• High levels of fats, particularly triglycerides, in the blood
These combined health problems appear to promote the deposit of fat in the liver. For some people, this excess fat acts as a toxin to liver cells, causing liver inflammation and nonalcoholic steatohepatitis, which may lead to a buildup of scar tissue (fibrosis) in the liver.
Risk factors include:
• Being overweight
• Having high blood fat levels, either triglycerides or LDL (“bad”) cholesterol
• Having diabetes or prediabetes
• Having high blood pressure
Complications
The main complication of fatty liver disease is the progression of NASH to cirrhosis. Cirrhosis means permanent scarring and hardening of the liver.
Prevention
To reduce your risk of nonalcoholic fatty liver disease:
• Choose a healthy diet. Choose a healthy plant-based diet that’s rich in fruits, vegetables, whole grains and healthy fats.
• Maintain a healthy weight. If you are overweight or obese, reduce the number of calories you eat each day and get more exercise. If you have a healthy weight, work to maintain it by choosing a healthy diet and exercising.
• Exercise. Exercise most days of the week. Get an OK from your doctor first if you haven’t been exercising regularly.
Diagnosis
Because nonalcoholic fatty liver disease causes no symptoms in most cases, it frequently comes to medical attention when tests done for other reasons point to a liver problem. This can happen if your liver looks unusual on ultrasound or if you have an abnormal liver enzyme test.
Tests done to pinpoint the diagnosis and determine disease severity include:
• Blood tests
• Complete blood count
• Liver enzyme and liver function tests
• Tests for chronic viral hepatitis (hepatitis A, hepatitis C and others)
• Celiac disease screening test
• Fasting blood sugar
• Hemoglobin A1C, which shows how stable your blood sugar is
• Lipid profile, which measures blood fats, such as cholesterol and triglycerides
Imaging procedures
Imaging procedures used to diagnose nonalcoholic fatty liver disease include:
• Plain ultrasound, which is often the initial test when liver disease is suspected.
• Computerized tomography (CT) scanning or magnetic resonance imaging (MRI) of the abdomen. These techniques lack the ability to distinguish nonalcoholic steatohepatitis from nonalcoholic fatty liver disease, but still may be used.
• Transient elastography, an enhanced form of ultrasound that measures the stiffness of your liver. Liver stiffness indicates fibrosis or scarring.
• Magnetic resonance elastography, which combines magnetic resonance imaging with patterns formed by sound waves bouncing off the liver to create a visual map showing gradients of stiffness throughout the liver reflecting fibrosis or scarring.